Can Cannabis Assist In Treating PTSD?
Numerous studies suggest possible benefits of using cannabis to treat PTSD, but results and conclusions are mostly incomplete or inconclusive. Marijuana’s classification as a Schedule 1 substance makes it difficult for researchers to gain access to medical cannabis and conduct exhaustive studies. Consequently, studies on the use of cannabis to treat PTSD are mainly anecdotal, lack statistical data, neglect to control confounding factors, or excessively rely on self-reports. Many studies are conducted as observational or with bias and serve as a foundation for further exploration rather than providing objective evidence or conclusions.
A report published by the National Academies of Sciences, Engineering and Medicine concluded the following:
- There is no evidence to support or refute that cannabis use increases the risk of PTSD.
- There is moderate evidence for an association between CUD and PTSD.
- There is limited evidence for increased symptom severity among individuals with PTSD.
A recent 2019 study determined that there is “insufficient evidence to support the use of cannabinoids as a psychopharmacological treatment for PTSD,” but acknowledged that, due to significant clinical need, future research is warranted to weigh the harms and benefits. The study seemed mostly concerned with the push to adjust policy making regarding cannabis without proper evidence to attest to the benefits. The study emphasized that clinical effectiveness is presently hypothetical rather than disparaging the idea that cannabis can treat PTSD.
Considering the already dangerous side-effects of current psychopharmaceuticals, the comparatively minimal and less perilous side-effects of cannabis and an apparent urgency for PTSD solutions, veterans suffering from PTSD should strongly consider cannabis as part of their treatment program if their symptoms are severe or unresponsive to treatment.
CBD vs. THC
Though cannabis contains over 70 distinct compounds, valuable insights have been discovered regarding the prominent components, THC and CBD. To take advantage of THC, the primary psychoactive component of marijuana, growers have been developing new strains with increasing THC levels over the years. However, recent studies have been highlighting CBD, the most abundant and non-psychoactive compound, as the most beneficial for medicinal purposes.
While THC is associated with the “high” and “active” effects of marijuana, CBD may produce antipsychotic and anxiolytic effects that counteract THC’s harmful components. Additionally, CBD may be useful in modulating fear-related symptoms of PTSD, such as the creation and maintenance of traumatic memories. The administration of CBD products after a traumatic event could help deter fear-induced memory processing.
Possible Benefits of Treating PTSD With Cannabis
The ability of cannabis to influence the body’s endocannabinoid system may make it invaluable for managing three of the core components of PTSD: reexperiencing, avoidance and numbing, and hyperarousal. Preclinical evidence supports the notion that CBD is an effective treatment when administered acutely for symptoms such as:
- Sleep disorders and disturbances.
- Emotional regulation.
- Stress tolerance.
One study showed a greater than 75% reduction in CAPS symptom scores (a universal method of measuring PTSD) when patients used cannabis compared to when they did not. Another study reported that some patients benefited from reduced anxiety and insomnia and improved coping abilities. Additional findings suggest that cannabis may even be capable of preventing PTSD symptoms in the first place when administered shortly after a traumatic event.
Cannabis-use is most helpful and least problematic for those using it for physical symptoms such as chronic pain. Individuals reported that cannabis was moderately to mostly beneficial, though less than half of those reported a reduction in corresponding symptoms.
We do have the potential, however, to do better than just treating symptoms of PTSD via activation of the cannabinoid receptors. With the right combination of extinction/habituation therapy and the judicious administration of a FAAH inhibitor like KDS-4103 we have the potential to actually cure many cases of PTSD.
Dr. Raphael Mechoulam, Ph.D.
Possible Dangers of Treating PTSD With Cannabis
Abusing marijuana can trigger predisposing conditions such as depression, anxiety, and psychosis. Though a traumatic event must trigger PTSD, other mental conditions can intensify the symptoms of PTSD. Following, as with opioids and alcohol, marijuana may provide temporary relief while worsening symptoms like depression and anxiety over time. Moreover, if the brain becomes dependent on a drug to balance its neurotransmitter chemistry, it could lead to a deficit of dopamine or serotonin.
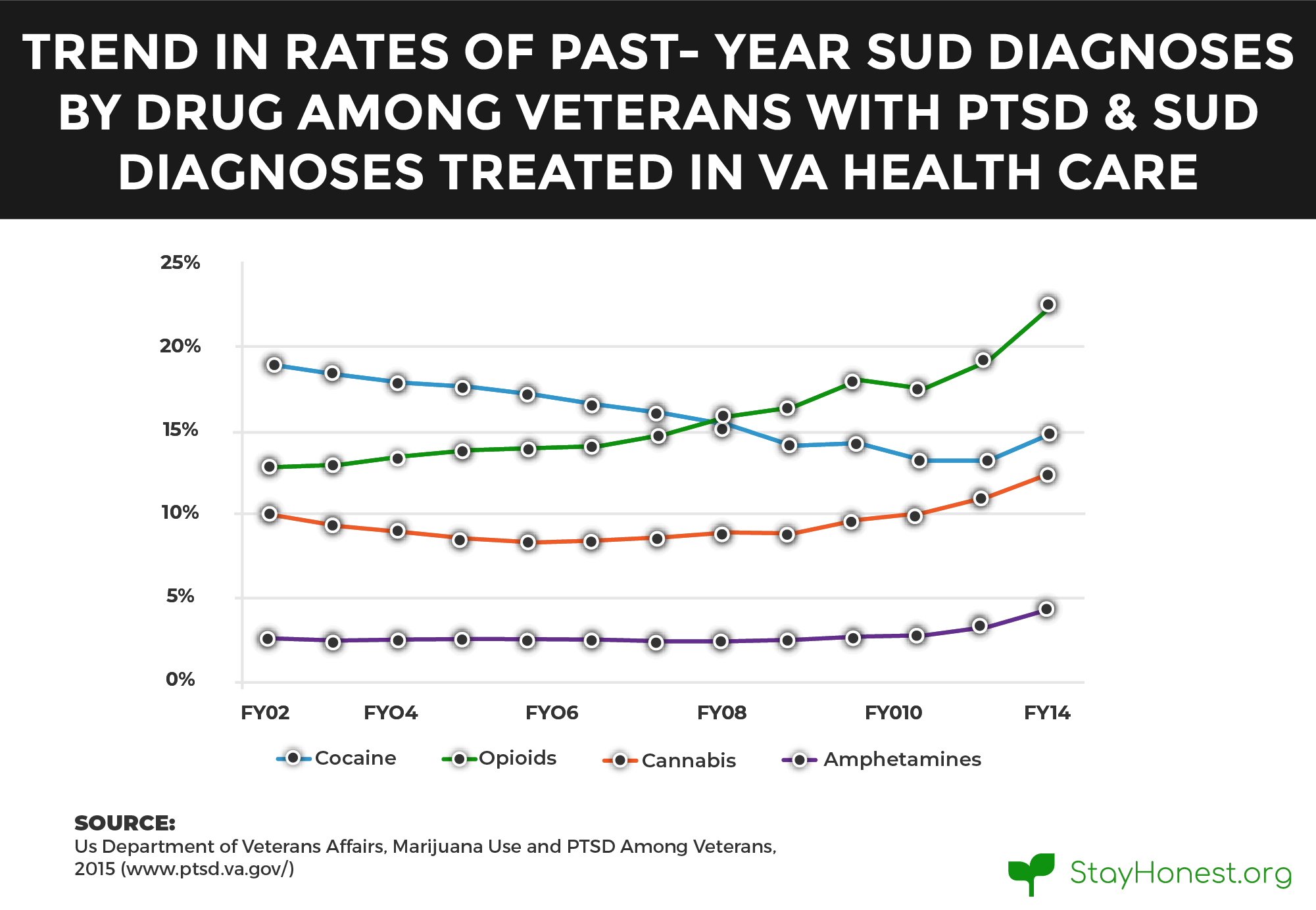
A VA study corroborated that cannabis provides short-term relief with possible long-term, harmful side-effects. Veterans with PTSD have a greater availability of cannabinoid type I receptors in the brain, which cannabinoids from marijuana will artificially bind to. This provides short term alleviation of stress symptoms associated with PTSD, but long-term use may create tolerance, causing the receptors to require more marijuana to function.
In this observational study, initiating marijuana use after treatment was associated with worse PTSD symptoms, more violent behavior and alcohol use. Marijuana may actually worsen PTSD symptoms or nullify the benefits of specialized, intensive treatment.
Samuel Wilkinson, MD, Yale School of Medicine
Barriers and Advances In Treating PTSD With Cannabis
While policies regarding medical and recreational cannabis use have been changing at the state level, federal law has yet to adapt or make allowances. Federal constraints do more than simply prevent recreational use; rather, they keep patients, health care professionals, and policymakers in the dark. The general public and institutions alike lack the information and evidence regarding the risks and benefits of cannabis, that they need to make informed decisions. The federal government continues to enforce restrictive policies and regulations on research. The main obstacles for urgently needed research are:
Investigators must go through a lengthy and complicated approval process before conducting research or studies. They must seek permission from a variety of federal, state, or local institutions, with layers of bureaucracy driven by the Schedule I categorization of cannabis.
Research cannabis is only available through the National Institute on Drug Abuse’s (NIDA) Drug Supply Program, which primarily focuses on the consequences of drug use and addiction. The NIDA is committed to ensuring public safety rather than pursuing research in potential applications.
Without adequate financial support, it is difficult for researchers to conduct thorough or lengthy studies. In 2015, only 16.5 percent ($10,923,472) of the NIDA budget for cannabinoid research supported studies that explored the potential benefits of therapeutic cannabis use—despite growing evidence that cannabis may have curative properties.
The VA’s Formal Stance
The VA’s policy does not currently endorse the use of cannabis to treat PTSD and will not pay for medical marijuana prescriptions. VA clinicians may only prescribe medications that have been approved by the U.S. Food and Drug Administration (FDA) for medical use, which presently does not include most products that contain THC, CBD, or other cannabinoids. VA clinicians are also not allowed to recommend medical marijuana to their patients.
You can, and are encouraged, to discuss the use of medical cannabis with your VA provider. Health care providers will record cannabis use in their medical records; however, records are confidential and protected under patient privacy and confidentiality laws and regulations. Most importantly, you will not be denied VA benefits because of marijuana use.
The VA Medical Cannabis Research Act of 2018 authorized the VA to conduct and support research on medical cannabis, including for veterans enrolled in the VA health care system with conditions such as chronic pain or PTSD, suggesting that current medical marijuana policies are subject to future developments.
First Ever Clinical Trial
Recent efforts have been made to advance our understanding of cannabis and its medical uses. The Multidisciplinary Association for Psychedelic Studies (MAPS) completed the first-ever clinical trial on smoking marijuana to combat veterans’ PTSD symptoms. The U.S. Public Health Service approved of the study in 2014, and after denying MAPS access to medical marijuana for developmental research for over 22 years, the Drug Enforcement Administration (DEA) announced their intention to grant licenses to additional marijuana growers for research. The study, which began in 2017, completed its treatment phase in January 2019, and the publication of the results is eagerly anticipated.
Resources for Veterans and Their Loved Ones
Dealing with the symptoms of PTSD can be challenging for victims and family members. The first step to recovery is seeking help—a little support can go a long way. Whether you are interested in cannabis treatment or alternative solutions, check out the links below for information and aid.
VA PTSD Treatment Programs
All VA medical centers offer treatment for PTSD; however, you can search by state for programs dedicated explicitly to PTSD. VA services are provided to all veterans who:
- Completed active military service in the Army, Navy, Air Force, Marines, or Coast Guard (or Merchant Marines during WWII).
- Were discharged under other than dishonorable conditions.
- Were National Guard members or Reservists who have completed a federal deployment to a combat zone
Veterans Crisis Line
If you are a veteran in a crisis or concerned about a loved one who is, connect with the crisis line via phone call, online chat, or text to reach caring, qualified responders from the VA.
Treatment Decision Aid
This decision aid helps you make important decisions regarding PTSD treatment. Along with basic information on PTSD, you can compare treatment options and take the next steps to find a provider.
Find a Therapist
The VA’s informational page on finding a therapist, counselor, or mental health care provider who can help with recovery. Includes steps as well as ways to find a provider using the internet or by phone.
PTSD Coach
This mobile phone application from the VA can help you learn about and manage PTSD symptoms.
Self-help and Coping
Learn to deal with excessive stress levels after trauma and other self-help strategies.
The first thing a family member needs to think about is: this is not your fault. This is something that has happened to your [loved one] that they don’t always have control over… It is not something that you need to be ashamed of.
Florence Vaught, Wife of a Veteran with PTSD
Resources for Medical Cannabis
Patients looking to try medical cannabis will have to look to non-government resources. Fortunately, there are reputable organizations that educate and help people gain access to medical cannabis. If you are interested in cannabis as a treatment for PTSD, check out the following resources.
Finding a Treatment Center Near You
The process of finding nearby treatment centers is made easy with the following interactive map, based on SAMHSA’s facility locator: